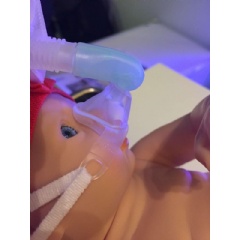
New noninvasive ventilation strategy allows preterm infants to breathe freely
Nasal high-frequency oscillatory ventilation reduces reintubation by more than 50 percent in high-risk preterm infants, according to a new study in the journal CHEST®
Preterm infants with respiratory distress syndrome (RDS) face heightened risks of death, critical illness, and prolonged hospitalization, particularly if they progress to develop acute respiratory distress syndrome (ARDS). A new studyappearing in the journal CHEST®, published by Elsevier, suggests that treatment with nasal high-frequency oscillatory ventilation (NHFOV) is a beneficial management strategy in this population, and is superior to nasal continuous positive airway pressure (NCPAP) in preventing reintubation.
“To our knowledge, this is the first study comparing NHFOV with NCPAP as postextubation respiratory support modes in preterm infants with neonatal ARDS,” explained lead investigator Yuan Shi, PhD, MD, FAAP, Department of Neonatology, Children’s Hospital of Chongqing Medical University, Ministry of Education Key Laboratory of Child Development and Disorders, Chongqing, China. “Usually, one of the most important causes of reintubation is difficulty in clearing the partial pressure of carbon dioxide (PCO2). We found that NHFOV was superior to NCPAP in reducing PCO2 levels.”
Invasive ventilation remains one of the cornerstones of reducing neonatal mortality in preterm infants with RDS and ARDS. RDS refers to breathing problems usually caused by lung immaturity due to premature birth. ARDS is an emergency medical condition, usually with acute onset, with symptoms similar to those of RDS; it may be caused by “clinical insults” such as inhalation of toxic chemicals, inhalation of vomit or meconium, lung inflammation or injury, pneumonia, or septic shock. No matter what the cause of respiratory dysfunction, invasive ventilation can increase the risk of ventilator-associated lung injury, which may result in bronchopulmonary dysplasia (BPD) and subsequent neurologic impairment, especially in infants who require repeated or prolonged intubation. Therefore, early weaning from invasive ventilation is key to reduce these risks and is a primary goal for neonatalogists.
NCPAP is a widely used therapy to improve ventilation in preterm infants but is not successful in avoiding reintubation in all infants. The new NHFOV technique was anticipated to improve outcomes by combining the advantages of NCPAP with those of high-frequency oscillatory ventilation (HFOV). Like NCPAP, NHFOV is noninvasive, but it also offers improved CO2 removal and increased functional residual capacity. The superimposed oscillations of NHFOV are thought to help avoid gas trapping and upregulate mean airway pressure (MAP).
This was a single center, randomized, controlled trial that enrolled 206 preterm infants born at less than 37 weeks’ gestational age who were ready for extubation. The babies were randomized into two groups of 103 to receive either NHFOV or NCPAP treatment. Of these infants, 61.7 percent were diagnosed with RDS, 25.7 percent with ARDS, and 12.6 percent with both RDS and ARDS. Data were analyzed for the overall group, as well as for those who were preterm (born at 32-36 weeks’ gestation) or very preterm (less than 32 weeks’ gestation).
The rate of reintubation in the group receiving NCPAP was more than twice as high compared to infants who received NHFOV (34.0 percent vs 15.5 percent), especially in the very preterm group or those with ARDS or combined ARDS/RDS, but not in those with only RDS. After six hours of extubation, the PCO2 levels in infants treated with NHFOV were significantly lower than those treated with NCPAP.
Infants treated with NHFOV were also able to leave the hospital in fewer days than those who received NCPAP. The only adverse events reported in the NHFOV group were nasal trauma and intestinal dilation.
Two international randomized controlled trials are ongoing to establish the clinical superiority of NHFOV compared to other respiratory support methods for avoiding reintubation in this fragile group of preterm babies.
------
The article is “Nasal High-Frequency Oscillatory Ventilation in Preterm Infants With Respiratory Distress Syndrome and ARDS After Extubation: A Randomized Controlled Trial,” by Long Chen, PhD, MD; Li Wang, PhD, MD; Juan Ma, MD; Zhichun Feng, PhD, MD; Jie Li, MD; and Yuan Shi, MD, PhD (https://doi.org/10.1016/j.chest.2019.01.014). It appears in the journal CHEST®, volume 155, issue 4 (April 2019) published by Elsevier.
This study was supported by the Social Livelihood Program of Chongqing Science and Technology Commission, China (No. cstc2018jscx-msybX0040). Clinical Trial Registration: Registry name: Nasal High Frequency Oscillation Ventilation (NHFOV) for Respiratory Distress Syndrome. The present study has been registered at www.clinicaltrials.gov. ID: NCT03140891.
About the journal CHEST®
The journal CHEST, the official publication of the American College of Chest Physicians®, features the best in peer-reviewed, cutting-edge original research in the multidisciplinary specialties of chest medicine: pulmonary, critical care, and sleep medicine; thoracic surgery; cardiorespiratory interactions; and related disciplines. Published since 1935, it is home to the highly regarded clinical practice guidelines and consensus statements. Readers find the latest research posted in the Online First section each week and access series that provide insight into relevant clinical areas, such as Recent Advances in Chest Medicine; Topics in Practice Management; Pulmonary, Critical Care, and Sleep Pearls; Ultrasound Corner; Chest Imaging and Pathology for Clinicians; and Contemporary Reviews. Point/Counterpoint Editorials and the CHEST Podcasts address controversial issues, fostering discussion among physicians. Access the journal CHEST online at chestjournal.org.
About American College of Chest Physicians® (CHEST)
CHEST is the global leader in prevention, diagnosis, and treatment of chest diseases. Its mission is to champion advanced clinical practice, education, communication, and research in chest medicine. It serves as an essential connection to clinical knowledge and resources for its 19,000+ members from around the world who provide patient care in pulmonary, critical care, and sleep medicine. For information about the American College of Chest Physicians, and its flagship journal CHEST®, visit chestnet.org.
About Elsevier
Elsevier is a global information analytics business that helps scientists and clinicians to find new answers, reshape human knowledge, and tackle the most urgent human crises. For 140 years, we have partnered with the research world to curate and verify scientific knowledge. Today, we’re committed to bringing that rigor to a new generation of platforms. Elsevier provides digital solutions and tools in the areas of strategic research management, R&D performance, clinical decision support, and professional education; including ScienceDirect, Scopus, SciVal, ClinicalKey and Sherpath. Elsevier publishes over 2,500 digitized journals, including The Lancet and Cell, 39,000 e-book titles and many iconic reference works, including Gray’s Anatomy. Elsevier is part of RELX Group, a global provider of information and analytics for professionals and business customers across industries. www.elsevier.com
( Press Release Image: https://photos.webwire.com/prmedia/6/239978/239978-1.jpg )
WebWireID239978
This news content was configured by WebWire editorial staff. Linking is permitted.
News Release Distribution and Press Release Distribution Services Provided by WebWire.